
Blue Cross Blue Shield health plans across the country have already invested in Codoxo’s AI technology and are moving toward a future with fewer dollars lost to FWA and improved payment integrity.

Blue Cross Blue Shield health plans across the country have already invested in Codoxo’s AI technology and are moving toward a future with fewer dollars lost to FWA and improved payment integrity.
Helping Blues plans push the boundaries of what’s possible through AI technology and services.
NATIONAL BLUE PLAN
6+ Million Members
MIDWEST BLUE PLAN
2+ Million Members
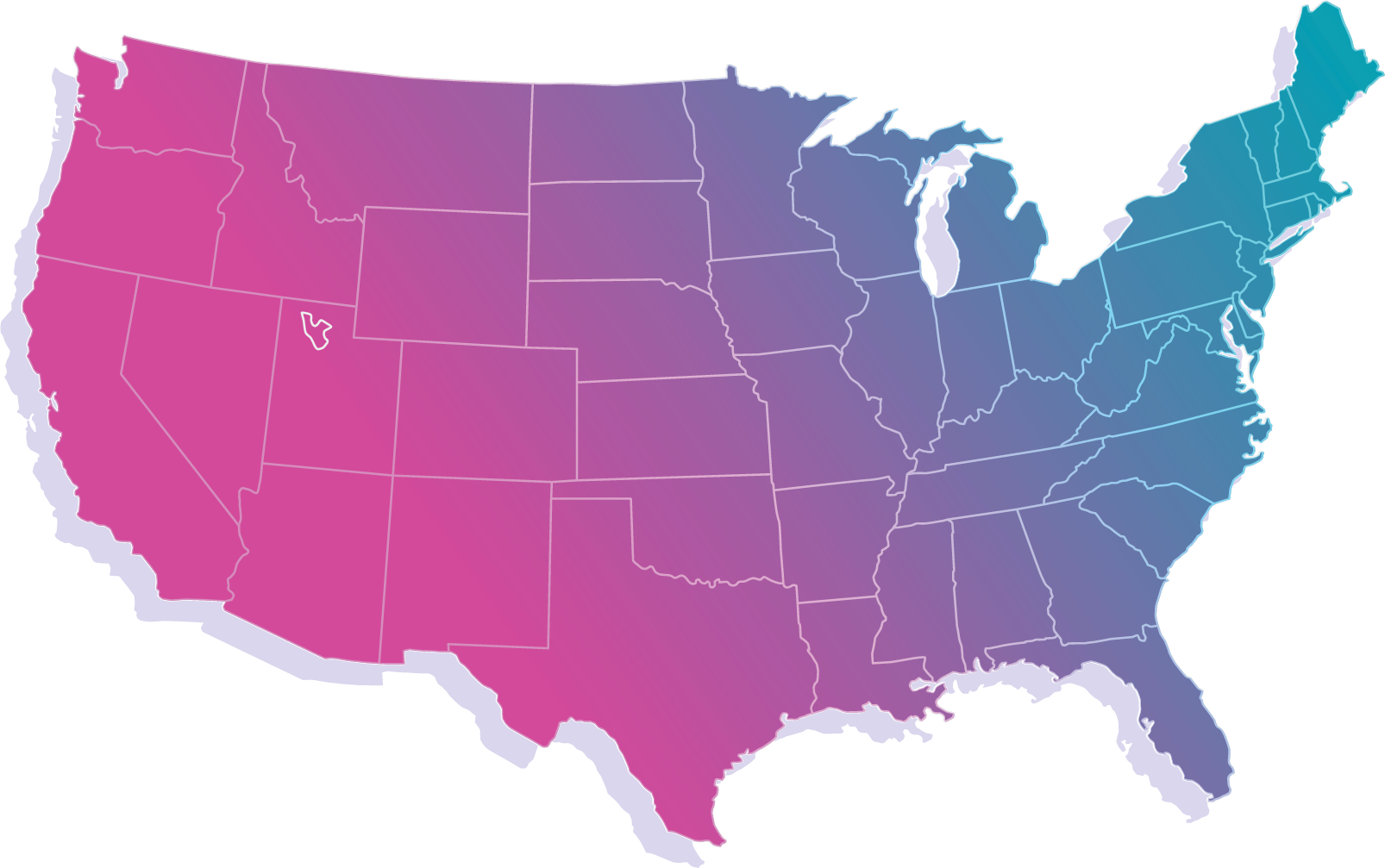
WESTERN BLUE PLAN
750+ Thousand Members
SOUTHEASTERN BLUE PLAN
800+ Thousand Members
SOUTHEASTERN BLUE PLAN
2.5+ Million Members
Highmark Identifies Millions in New Active Cases with AI-Powered Provider Analysis
Highmark’s Financial Investigation and Provider Review (FIHR) team uses Codoxo’s Fraud Scope platform in combination with rules-based systems to stay ahead of evolving schemes by identifying early patterns for suspect billing of medical services before big financial liability occurs.

Codoxo’s AI has identified millions of dollars in cases the FIPR team is actively investigating

A dedicated team reviews and prioritizes issues identified by Codoxo’s AI solution

Highmark plans to expand use of Codoxo’s Fraud Scope platform to the pre-pay stage to accelerate post-pay reviews and identify early signs of FWA
Western Blue Plan Identifies Projected Risk Exposure of over $2.2M in an 18-month Period
West coast-based Blues health plan used Codoxo’s Fraud Scope platform to identify and investigate a previously unknown fraud scheme that significantly impacted patient safety and created a projected risk exposure of over $2.2M in an 18-month period. The plan was able to detect the outlier provider behavior and quickly begin the investigation process for rapid intervention.
Codoxo’s Fraud Scope platform captures approximately 97% of total post-payment exposures for a Blues health plan
A large national health plan uses Fraud Scope, along with many other tools/sources to monitor existing and emerging FWA schemes on an ongoing basis. After years of using the platform in conjunction with these other tools, Codoxo conducted a comparative study to determine the level of accuracy if Fraud Scope had been the only tool used in identifying post-payment exposure for the plan.
Here’s what we found.

of total post-payment exposures were identified by Fraud Scope alone

of additional leads and exposures were identified and not caught by the plan’s other solutions

of egregious providers were flagged to help the plan prioritize the highest exposures first
“With Codoxo, we have a true partnership and collaboration for the common good.”
J.R. Trevino, Manager, Special Investigations Unit, Driscoll Health Plan
